
Artificial intelligence in surgery: use cases and challenges


Surgery's about to get a high-tech facelift, with artificial intelligence surgery projected to elevate the number of global surgical procedures to an estimated 373 million by 2030, as reported by Next Move Strategy Consulting. This surge in AI-assisted surgery is set to transform surgical care, enhancing efficiency, precision, and overall healthcare delivery from preoperative planning to post-op care.
With the WHO forecasting a shortfall of 10 million healthcare workers by 2030, AI's role in surgery becomes even more crucial. AI in robotic surgery promises to fill this gap and propel the surgical robotics market toward $21.41 billion by 2030. Additionally, AI's diagnostics capabilities significantly reduce unnecessary surgeries, with one study highlighting a drop in error rates for detecting cancerous lymph nodes from 3.4 to 0.5 percent.
Yet, AI software development in healthcare has its obstacles. Eugene Kruglik, Vention expert in healthcare technology solutions, highlights a major hurdle: "One of the primary AI challenges is the lack of data, which can render an AI system ineffective, as it needs a vast number of images and videos for training."
Let's delve deeper into the AI in surgery use cases and challenges, as well as explore what benefits AI brings to the (operating) table.

Shape your AI transformation with a scalpel, not a sledgehammer.
Vention’s State of AI 2026 report brings market data, major industry moves, and focused insights to help you build on what you already have.
How AI can be integrated into each phase of surgery
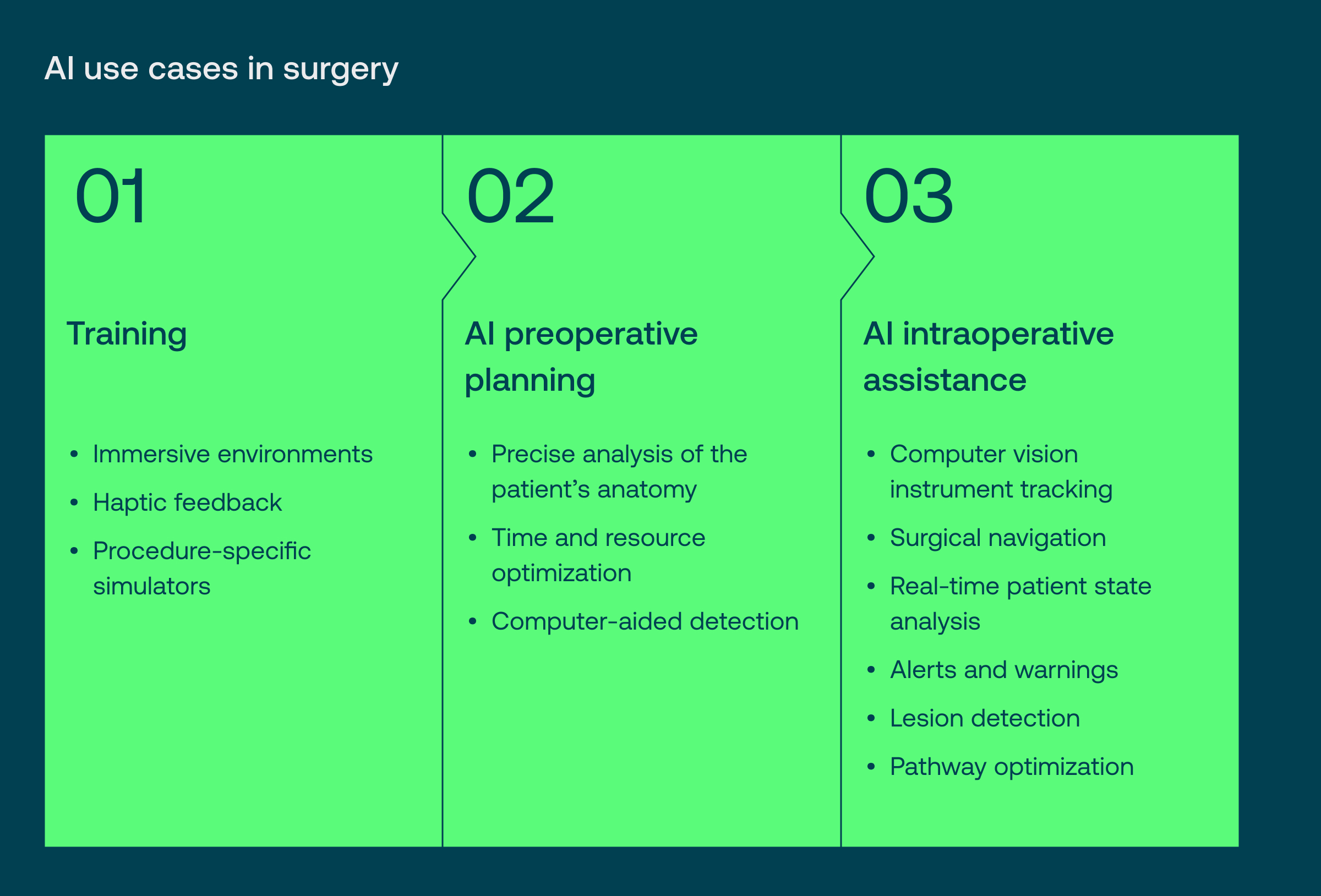
AI surgical training
The Joint Commission analyzed 1,441 significant medical mishaps and discovered that surgeries performed on the incorrect body part comprised six percent of these incidents. The root of this issue often lies in inadequate medical education and the selection of inappropriate treatments.
Implementing AI technology is an effective strategy to improve the accuracy and safety of surgical practices.
Immersive environments
VR in surgery training excels on its own, but pairing it with AI can significantly enhance the fidelity and customization of surgical simulations. These AI-enhanced VR simulations provide highly accurate reproductions of surgical procedures, detailed anatomical models, and realistic interactions with surgical instruments. Plus, each simulation can be adjusted to the surgery's complexity and the learner's proficiency level.
Haptic feedback
Haptic feedback technology offers trainees a true-to-life feel during simulated surgeries by mimicking tissue resistance, incisions, and interaction with surgical tools. It also simulates various medical conditions, helping learners understand the differences in tissue characteristics.
AI also assesses how users handle surgical instruments, paying attention to the angle, pressure, and precision of their movements. The technology can even introduce unexpected scenarios, such as bleeding or unintentional tissue damage, enhancing the realism of the simulation.
Procedure-specific simulators
AI customizes simulations for specific surgical procedures, such as knee replacements or appendectomies, capturing the exact sequence of steps, challenges, and anatomical details. These simulations use AI algorithms to guide trainees through each phase of the surgery, advising on the correct instruments and incision techniques.
Trainees receive immediate feedback on their accuracy, speed, and adherence to surgical protocols. What’s more, AI applications adjust the difficulty level of simulations based on the learner's proficiency, ensuring that the training remains consistently challenging and effective.

AI preoperative planning
Precise analysis of the patient’s anatomy
AI algorithms assist surgeons in accurately preparing for operations by segmenting medical images from CT scans, MRIs, or X-rays. This technology leverages machine learning, particularly deep learning techniques like convolutional neural networks (CNNs), which are trained on vast libraries of labeled medical imagery.
AI models can easily isolate specific anatomical structures or areas of interest and create detailed maps of a patient's anatomy, including organs, blood vessels, tumors, and other anomalies.
A groundbreaking 2023 study by University of Copenhagen researchers demonstrated that combining a diagnostic AI system and mammographic texture analysis surpasses conventional models in predicting short-term and long-term breast cancer risks.
Time and resource optimization
A forecast from the Association of American Medical Colleges predicts a shortfall of 15,800 to 30,200 surgeons in the US by 2034.
In this context, AI algorithms emerge as a crucial tool. They can navigate through patient data — from medical histories to the urgency of medical procedures—to streamline scheduling and prioritize surgeries based on clinical needs.
AI models evaluate various factors, including the complexity of surgeries, the proficiency of surgeons, and the need for specific equipment, ensuring a seamless operational flow.
Computer-aided detection (CAD)
In 2022, the market for computer-aided detection was valued at $818.5M and is projected to expand at a CAGR of 5.9 percent by 2030.
When enhanced by AI, CAD offers detailed analysis of pathological tissues, helping to understand their density, composition, and blood supply. It plays a crucial role in assessing tumor boundaries and enables surgeons to determine the necessary scope of cancer tissue removal.
CAD provides precise measurements of tumors and their proximity to vital organs, facilitating targeted surgery and minimizing the likelihood of leaving behind cancerous cells.
AI intraoperative assistance
Computer vision-enabled instrument tracking
Computer vision allows for real-time monitoring of surgical tools during operations, allowing surgeons to focus on the most crucial parts of the surgery with confidence that the system is accurately tracking the tools.
AI-powered tracking is particularly beneficial in minimally invasive surgeries (MIS), where visibility is limited. It effectively addresses challenges associated with smaller incisions and restricted viewing angles.
Surgical navigation
During surgery, AI acts as a smart assistant, providing real-time assistance and guidance by continuously monitoring the surgical process for any changes. Surgeons can immediately adjust their approach if the surgical field situation evolves or unforeseen changes arise.
AI's ability to adapt to real-time changes supports better decision-making, potentially reducing the risk of complications and improving patient outcomes.
Real-time patient state analysis
Similar to its role in surgical navigation, AI helps monitor the patient's physiological state — heart rate, blood pressure, and oxygen saturation — during operations. The AI system integrates data from medical devices and electronic health records (EHRs), providing real-time patient condition updates with actionable recommendations.
During anesthesia procedures, AI offers continuous feedback to the anesthesia team. It evaluates the patient's response to anesthesia drugs in real-time, enabling precise dosage adjustments for optimal patient comfort and safety.
Alerts and warnings
AI algorithms identify anomalies in monitored data (think fluctuations in vital signs, unexpected events, or deviations from the surgical plan). Upon detecting an anomaly, the AI system generates immediate alerts. These notifications are sent to the surgical team via visual cues, auditory signals, or other communication channels to prompt immediate action.
Lesion detection
AI algorithms can process images from surgical cameras and endoscopes in real-time, pinpointing and highlighting lesions in the surgical area. By incorporating various imaging techniques, such as intraoperative ultrasound, fluorescence imaging, and multispectral imaging, AI enhances the accuracy of lesion detection throughout surgical procedures.
Pathway optimization
With pathway optimization, doctors can consider individual patient characteristics, anatomical differences, and potential complications to choose the best surgical approach. Unique algorithms analyze extensive data to determine the most effective surgical routes.
The impact of AI on decision support and data research for surgeons
Beyond training, planning, and execution, AI is a game-changer in surgical decision-making and analysis.

Decision support systems
Decision support systems can be used before, during, and after operations to assist medical professionals with diagnosis, treatment planning, surgical navigation, and post-operative care.
Such AI systems collect essential information about the patient and the surgical procedure and analyze this data using machine learning algorithms. The result is valuable insights that help assess risks, create treatment plans, and predict possible treatment outcomes.
|
Input |
Output |
|
| Customized risk evaluation |
|
|
| Personalized treatment plans |
|
|
| Operation’s outcome prediction |
|
|
Data analysis and research
AI holds immense potential in research and promises improved outcomes in surgical procedures.
Big data analytics and population studies
AI streamlines collecting and integrating various data types, such as EHRs, imaging, and genomic information, offering a holistic view of patient groups. It employs algorithms to detect patterns and insights within these large datasets, such as demographic trends and disease patterns, which might be difficult to discern through conventional analysis.
AI also supports population health management by identifying at-risk demographics, suggesting preventive actions, and improving the distribution of healthcare resources. Additionally, AI-powered analytics enhance epidemiological research by examining disease prevalence and causes across populations.
NLP text mining tools
The healthcare industry increasingly embraces natural language processing (NLP) due to its capabilities across searching, analyzing, and interpreting vast patient datasets.
Several noteworthy examples of NLP use in surgery include:
- Semantic search and information retrieval
AI enhances the ability to conduct semantic searches across medical databases, allowing healthcare professionals to find relevant information based on the meaning and context of their queries. This is particularly useful for researching specific surgical techniques, outcomes, or case studies.
- Literature review and knowledge discovery
AI can automate the review of extensive surgical literature and research, enabling the discovery of new insights and trends in surgical practices. By analyzing patterns and outcomes in existing studies, AI helps identify effective surgical techniques and potential areas for innovation, making it easier for surgeons to stay updated with the latest advancements.
- EHR analysis
AI algorithms can sift through EHRs to extract and analyze patient data relevant to surgical procedures, including preoperative assessments, previous surgeries, and postoperative outcomes.
- Extraction of surgical parameters
AI tools can automatically extract important parameters from surgical data, such as operation duration, blood loss, or surgical instrument types. This information is crucial for analyzing surgical efficiency, comparing different surgical approaches, and improving surgical protocols and guidelines.

AI robotic surgery systems
Let’s explore the leading AI-assisted surgery systems for minimally invasive procedures that empower surgeons to perform precise, flexible, and enhanced operations.
Intuitive's Da Vinci AI-assisted robotic surgery systems, particularly the Da Vinci Xi and Da Vinci X models, are prime examples of AI in surgery.
The Da Vinci Xi is renowned for its advanced instrumentation, Firefly fluorescence imaging for better visualization of vessels and tissue perfusion, and integrated table motion. Alongside the Da Vinci X, these systems represent the pinnacle of surgical precision, vision, and control.
The advanced AI integration in Da Vinci systems allows for accurate image analysis, surgical planning, and dynamic adjustments tailored to each patient's unique anatomical and physiological profile. These personalized enhancements elevate surgical outcomes, improve patient experiences, and expedite recovery.
The Senhance Surgical System is another example of AI in surgery; it combines AI technology with surgical expertise to counteract the effects of surgeon fatigue. This system makes the cost and duration of operations comparable to traditional laparoscopy, expanding access to advanced minimally invasive surgeries.
Featuring robotic precision, haptic feedback, eye-tracking camera control, enhanced ergonomics, and an open-platform architecture, Surgeons can perform complex procedures with greater precision and control, reducing human error and improving patient outcomes.
Versius offers surgeons unparalleled flexibility in choosing the most advantageous port placements, merging traditional laparoscopy techniques with the advanced capabilities of AI-assisted robotic surgery. Its open design promotes seamless communication among surgical teams, ensuring cohesive and efficient operations.
With fully-wristened instruments and superior 3D HD visualization, Versius equips surgeons to easily navigate intricate anatomical areas.
The Hugo™ RAS system, designed by surgeons for surgeons, introduces significant flexibility and adaptability, fitting various operating room environments and meeting the demands of diverse procedures and patients.
Its integration of Touch Surgery™ Enterprise provides robust video recording capabilities, allowing surgeons to review and refine their techniques remotely and elevate proficiency across distances.
The Hugo™ RAS system is accessible and scalable, lowering barriers to entry in terms of cost and maximizing operational efficiency and utilization rates.
Challenges and limitations of AI in surgery
AI will never replace physicians, given its inherent limitations. Yet, understanding these limitations can help us tackle the current AI challenges AI challenges medical specialists face.
Data limitations
Some might think it’s just the AI-enhanced program that assists surgeons in the operating room. The truth is, it’s data that helps AI thrive and innovate operations. Yet, researchers caution that we might either face a shortage of the data required for AI or run into storage capacity issues.
Considering the pivotal role of data in healthcare, whether AI is involved or not, it can introduce several challenges, particularly in AI surgery technology.
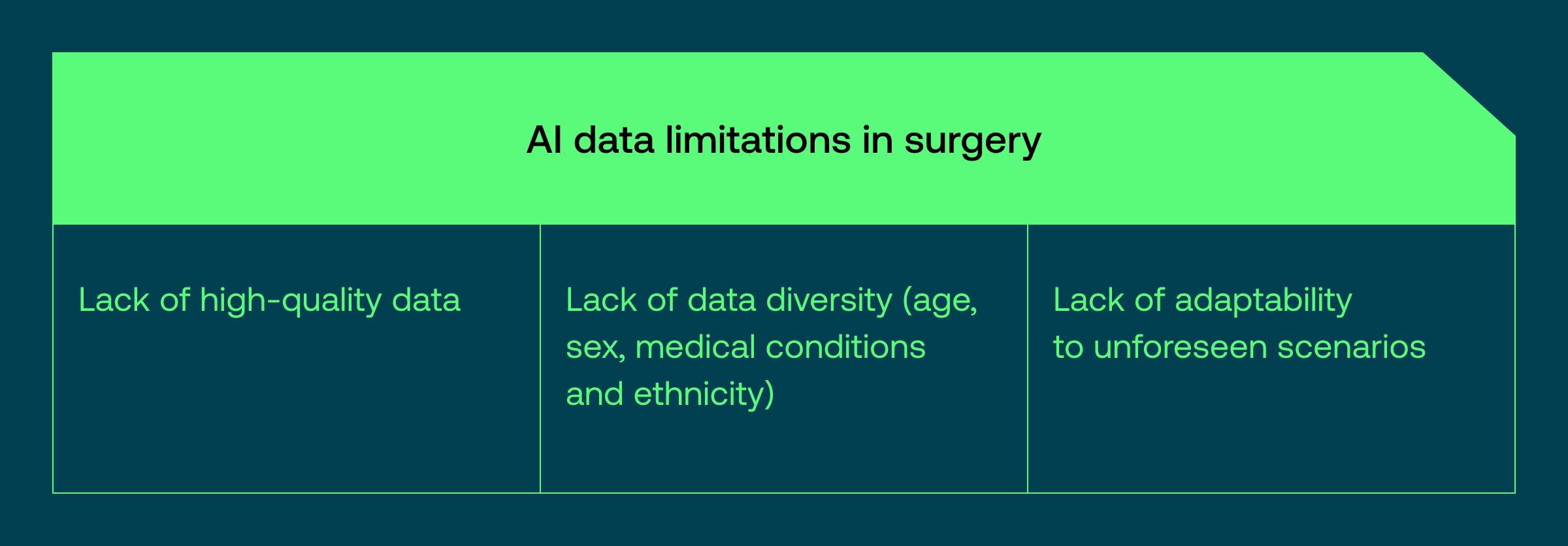
Lack of high-quality data
One of the main challenges of integrating AI for surgery is limited data sets and issues with the quality and consistency of this data. Finding the right data to train AI, especially for intricate surgical maneuvers, is like looking for a needle in a haystack — it’s scarce and demands significant resources.
Add to that the ever-changing clinical landscapes and shifts in data trends over time, and you face a real challenge in developing AI models that can stand the test of time and variability.
Eugene Kruglik highlights, "When clients approach us for AI development in healthcare, we first ask to see their data sets. Without access to high-quality data, we're skeptical about the AI models' quality, which could lead to serious, irreversible mistakes."
Lack of data diversity
Data challenges go beyond quality; they also involve ensuring datasets reflect the diverse populations they aim to serve, including variations in age, sex, medical conditions, and ethnicity.
The reason? When certain groups or medical conditions are underrepresented, it distorts AI models, leading to unequal service across different demographics. This lack of representation can cause these algorithms to underperform for those not adequately represented, potentially widening gaps in healthcare equality.
Addressing this requires deliberately sourcing diverse data, aiming for fair representation, and using techniques like data augmentation to develop AI models that perform well across various demographics and medical situations.
Lack of adaptability
One challenge of integrating AI into the operating room is its difficulty in handling unexpected situations. Since AI learns from historical data, it can be thrown off by new or unfamiliar scenarios.
To address this, it’s essential to continually update AI with diverse data that encompasses various possibilities. Additionally, enabling AI to learn in real-time and gather feedback during operations could significantly enhance its ability to manage unforeseen events.
This challenge is similar to the broader issue with AI surgery technology: Finding the right data is difficult, especially with the ever-advancing and constantly evolving medical field.
Opaque AI decision-making
The challenge with AI performing surgery isn't just about the data sets that form the foundation of any AI model; it's also about making its decisions clear to those who hold the scalpel. Surgeons and healthcare professionals often struggle to understand why AI makes certain recommendations, which can hinder trust in this technology.
Without clear insight into the “AI's thought process,” convincing clinicians to incorporate AI tools into their daily work becomes challenging. They need to know the “why” behind AI's advice as much as the “what.”
To bridge this gap, we need AI that performs and explains itself — creating models with features that make their decisions understandable. It's about fostering dialogue between the technicians behind AI and the medical professionals using it, ensuring the latter feel as confident about AI's decisions as they do about their own clinical judgments.
Now, AI companies are pulling back the curtain to reveal the magic behind AI models. Take our partner Comet, for example — they're revolutionizing how AI is trained, ensuring precise and transparent decisions.
Ethical and legal concerns
When connecting AI and surgery, the stakes are high: Ensuring patients are fully informed, protecting their privacy, and addressing biases in the algorithms are critical. Clarifying how AI makes decisions and establishing accountability when things go wrong is essential in building trust in AI-enhanced surgeries.
Pavel Nekrasov, the ML engineering manager at Vention, suggests: "Sticking to regulations, establishing clear rules on data ownership, and keeping a human in the loop are crucial for navigating the ethical and legal challenges of AI in surgery."
Loss of surgical skills
A significant concern is that over-reliance on AI could diminish surgical skills. It's crucial to find the right balance, using AI as an aid while continuing to develop hands-on surgical abilities.
Training and ongoing education must effectively integrate AI as a complement — not a substitute — to prevent the erosion of surgical skills. This approach ensures that healthcare professionals maintain their fundamental skills and precise touch.

AI for surgery: a supportive tool, not a replacement
As AI becomes a staple in operating rooms, it's essential to grasp two fundamental truths: Sophisticated AI applications are inevitable, and mastering AI surgery technology will be as crucial for surgeons as mastering the scalpel.
However, surgeons and healthcare professionals often struggle to understand the logic behind AI decisions, leading to decreased confidence in these technologies. This lack of transparency hinders the adoption of AI tools in medical settings, as practitioners typically seek straightforward justifications for the algorithm's suggestions.
Plus, while AI excels in data analysis and can enhance surgical precision, it lacks the adaptability and intuition to manage atypical cases. AI cannot provide concrete diagnoses or tactile insights from physical examinations. Excessive reliance on automated tools could erode a surgeon's skills in specific techniques, mainly if there is too much dependence on AI support.
Additionally, there are challenges with the limitations and underrepresentation in AI datasets, including their quality. "When clients approach us for AI development, our initial step involves analyzing video samples to eliminate smoke from the footage. This enhances our ability to detect irregularities in images and videos, leading to improved diagnoses and ultimately lightening the physicians' workload," explains Eugene Kruglik.
By recognizing these AI challenges and focusing on developing transparent, supportive AI tools, we can enhance the effectiveness of AI surgery technology and software as a medical device solutions, ensuring they elevate rather than overtake human expertise.
Need AI experts for your next healthcare project?
Our consultants are ready to advise you on building an efficient, scalable, compliant, and cost-effective solution.






